


Medi-Cal renewals have resumed, and millions of individuals may lose health coverage. They will need to take action to either keep their current Medi-Cal coverage or find a new health plan that’s right for them. There are options to make sure they stay covered and protected. We can help.
You may have employees who waived employer-sponsored health coverage and kept their Medi-Cal benefits when starting employment with your company.
If these employees are disenrolled from Medi-Cal, they may become eligible for a special enrollment period due to what’s known as a qualifying life event. During this specified window of time, employees can enroll in a group medical plan or obtain other health coverage outside of your organization’s standard open enrollment period.1
An employee may not qualify for either Medi-Cal or your group plan, but could enroll in an Anthem Individual and Family Plan or coverage through Covered California™.



Bill was hired as a part-time employee and not eligible for employer-sponsored coverage. Bill has diabetes, and having health coverage to manage his condition is important. He enrolled in Medi-Cal at a time when state eligibility reviews were paused. Now his position has been moved to full-time status.
With the restart of Medi-Cal eligibility reviews, Bill is notified that he is no longer eligible for Medi-Cal as his income has changed.
Bill relies on his diabetes management plan with his doctor, and staying covered is important to him. He reaches out to his company’s Human Resources (HR) department to discuss his plan options.
HR provides Bill coverage options to help determine what plan is best for him. He can choose to either enroll in his company’s group health plan or opt for an Anthem Individual and Family plan through Covered California.
Bill decides to join his company’s employer-sponsored health plan.
Since losing Medi-Cal coverage is a qualifying event with a special enrollment period, Bill is eligible to sign up during that period.
Click on the thumbnails to view the resources linked below.


1 Guidance may be issued at a later date extending the Special Enrollment Period in some circumstances.
2 Gallop®: Leaders: Ignore Employee Wellbeing At Your Own Risk (accessed September 2023): gallop.com.
3 Bill’s story represents a potential member journey and is hypothetical in nature.
4 The White House: Fact Sheet: Biden Harris Administration Proposes Rule to Fix “Family Glitch” and Lower Health Care Costs (accessed October 2022): whitehouse.gov.
Anthem Blue Cross is the trade name of Blue Cross of California. Independent licensee of the Blue Cross Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc.
1044513CAEENABC Rev. 2/24
Your employees have options for health insurance if they don’t qualify for your employer group plan. Our decision support tool can help them find the right health plan. The tool also offers personalized guidance by matching an employee to state and federal benefits they may qualify for, including food, housing, and child care programs.
Learn about the decision support tool here.



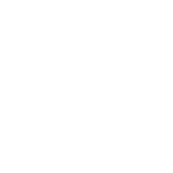
Employee coverage options flyer
Employee resources flyer
Printable information flyer
Health plan decision support tool flyer
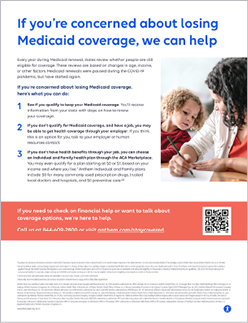
Employee coverage options website
Workplace communication template

An employee could still qualify for Medi-Cal benefits and maintain their coverage. Employees may take steps to renew coverage with their state agency.
An employee may no longer qualify for Medi-Cal benefits and could join your employer-sponsored group plan.
3


You may have employees who waived employer-sponsored health coverage and kept their Medi-Cal benefits when starting employment with your company.
If these employees are disenrolled from Medi-Cal, they may become eligible for a special enrollment period due to what’s known as a qualifying life event. During this specified window of time, employees can enroll in a group medical plan or obtain other health coverage outside of your organization’s standard open enrollment period.1
Medi-Cal renewals have resumed, and millions of individuals may lose health coverage. They will need to take action to either keep their current Medi-Cal coverage or find a new health plan that’s right for them. There are options to make sure they stay covered and protected. We can help.
Click on the thumbnails to view the resources linked below.
1
An employee could still qualify for Medi-Cal benefits and maintain their coverage. Employees may take steps to renew coverage with their state agency.
2
An employee may no longer qualify for Medi-Cal benefits and could join your employer-sponsored group plan.
3
An employee may not qualify for either Medi-Cal or your group plan, but could enroll in an Anthem Individual and Family Plan through Covered California.
Your employees have options for health insurance if they don’t qualify for your employer group plan. Our decision support tool can help them find the right health plan. The tool also offers personalized guidance by matching an employee to state and federal benefits they may qualify for, including food, housing, and child care programs.
With the restart of Medi-Cal eligibility reviews, Bill is notified that he is no longer eligible for Medi-Cal as his income has changed.
Bill was hired as a part-time employee and not eligible for employer-sponsored coverage. Bill has diabetes, and having health coverage to manage his condition is important. He enrolled in Medi-Cal at a time when state eligibility reviews were paused. Now his position has been moved to full-time status.
Bill relies on his diabetes management plan with his doctor, and staying covered is important to him. He reaches out to his company’s Human Resources (HR) department to discuss his plan options.
HR provides Bill coverage options to help determine what plan is best for him. He can choose to either enroll in his company’s group health plan or opt for an Anthem Individual and Family plan through Covered California.
Bill decides to join his company’s employer-sponsored health plan. Since losing Medi-Cal coverage is a qualifying event with a special enrollment period, Bill is eligible to sign up during that period.

Learn about the decision support tool here.


Making sure all of your employees are covered shows you support them prioritizing their health, and healthy employees are more focused and productive at work.



Employee coverage options flyer
Employee resources flyer
Printable information flyer
Health plan decision support tool flyer
Employee coverage options website
Workplace communication template
Your employees are the heart of your organization. As your trusted health partner, we can help you make sure they have the information they need to maintain health benefits and navigate changes in Medi-Cal coverage.


1 Guidance may be issued at a later date extending the Special Enrollment Period in some circumstances.
2 Gallop®: Leaders: Ignore Employee Wellbeing At Your Own Risk (accessed September 2023): gallop.com.
3 Bill’s story represents a potential member journey and is hypothetical in nature.
4 The White House: Fact Sheet: Biden Harris Administration Proposes Rule to Fix “Family Glitch” and Lower Health Care Costs (accessed October 2022): whitehouse.gov.
Anthem Blue Cross is the trade name of Blue Cross of California. Independent licensee of the Blue Cross Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc.
1044513CAEENABC Rev. 2/24


3