



Medicaid renewals have resumed, and millions of individuals may lose health coverage. They will need to take action to either keep their current Medicaid coverage or find a new health plan that’s right for them. There are options to make sure they stay covered and protected. We can help.
You may have employees who waived employer-sponsored health coverage and kept their Medicaid benefits when starting employment with your company.
If these employees are disenrolled from Medicaid, they may become eligible for a special enrollment period due to what’s known as a qualifying life event. During this specified window of time, employees can enroll in a group medical plan or obtain other health coverage outside of your organization’s standard open enrollment period.1


An employee could still qualify for Medicaid benefits and maintain their coverage. Employees may take steps to renew coverage with their state agency.
An employee may no longer qualify for Medicaid benefits and could join your employer-sponsored group plan.
An employee may not qualify for either Medicaid or your group plan, but could enroll in an Anthem Individual and Family Plan through the Health Insurance Marketplace® or their state exchange.



Bill was hired as a part-time employee and not eligible for employer-sponsored coverage. Bill has diabetes, and having health coverage to manage his condition is important. He enrolled in Medicaid at a time when state eligibility reviews were paused. Now his position has been moved to full-time status.
With the restart of Medicaid eligibility reviews, Bill is notified that he is no longer eligible for Medicaid as his income has changed.
Bill relies on his diabetes management plan with his doctor, and staying covered is important to him. He reaches out to his company’s Human Resources (HR) department to discuss his plan options.
HR provides Bill coverage options to help determine what plan is best for him. He can choose to either enroll in his company’s group health plan or opt for an Anthem Individual and Family plan through the federal Health Insurance Marketplace
or his state exchange.
Bill decides to join his company’s employer-sponsored health plan.
Since losing Medicaid coverage is a qualifying event with a special enrollment period, Bill is eligible to sign up during that period.
Click on the thumbnails to view the resources linked below.


1 Guidance may be issued at a later date extending the Special Enrollment Period in some circumstances.
2 Gallop®: Leaders: Ignore Employee Wellbeing At Your Own Risk (accessed September 2023): gallop.com.
3 Bill’s story represents a potential member journey and is hypothetical in nature.
4 The White House: Fact Sheet: Biden Harris Administration Proposes Rule to Fix “Family Glitch” and Lower Health Care Costs (accessed October 2022): whitehouse.gov.
Anthem Blue Cross and Blue Shield is the trade name of: In Colorado: Rocky Mountain Hospital and Medical Service, Inc. HMO products underwritten by HMO Colorado, Inc. In Connecticut: Anthem Health Plans, Inc. In Indiana: Anthem Insurance Companies, Inc. In Georgia: Blue Cross Blue Shield Healthcare Plan of Georgia, Inc. and Community Care Health Plan of Georgia, Inc. In Kentucky: Anthem Health Plans of Kentucky, Inc. In Maine: Anthem Health Plans of Maine, Inc. In Missouri (excluding 30 counties in the Kansas City area): RightCHOICE® Managed Care, Inc. (RIT), Healthy Alliance® Life Insurance Company (HALIC), and HMO Missouri, Inc. RIT and certain affiliates administer non-HMO benefits underwritten by HALIC and HMO benefits underwritten by HMO Missouri, Inc. RIT and certain affiliates only provide administrative services for self-funded plans and do not underwrite benefits. In Nevada: Rocky Mountain Hospital and Medical Service, Inc. HMO products underwritten by HMO Colorado, Inc., dba HMO Nevada. In New Hampshire: Anthem Health Plans of New Hampshire, Inc. HMO plans are administered by Anthem Health Plans of New Hampshire, Inc. and underwritten by Matthew Thornton Health Plan, Inc. In 17 southeastern counties of New York: Anthem HealthChoice Assurance, Inc., and Anthem HealthChoice HMO, Inc. In these same counties Anthem Blue Cross and Blue Shield HP is the trade name of Anthem HP, LLC. In Ohio: Community Insurance Company. In Virginia: Anthem Health Plans of Virginia, Inc. trades as Anthem Blue Cross and Blue Shield, and its affiliate HealthKeepers, Inc. trades as Anthem HealthKeepers providing HMO coverage, and their service area is all of Virginia except for the City of Fairfax, the Town of Vienna, and the area east of State Route 123. In Wisconsin: Blue Cross Blue Shield of Wisconsin (BCBSWI) underwrites or administers PPO and indemnity policies and underwrites the out-of-network benefits in POS policies offered by Compcare Health Services Insurance Corporation (Compcare) or Wisconsin Collaborative Insurance Corporation (WCIC). Compcare underwrites or administers HMO or POS policies; WCIC underwrites or administers Well Priority HMO or POS policies. Independent licensees of the Blue Cross and Blue Shield Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc.
1044513MUEENABS Rev. 2/24
Your employees have options for health insurance if they don’t qualify for your employer group plan. Our decision support tool can help them find the right health plan. The tool also offers personalized guidance by matching an employee to state and federal benefits they may qualify for, including food, housing, and child care programs.
Learn about the decision support tool here.


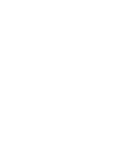
Employee coverage options flyer
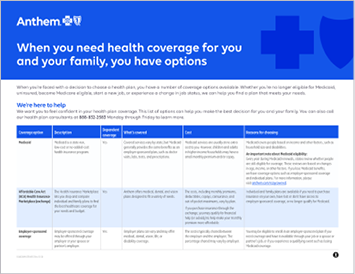
Employee resources flyer
Printable information flyer
Health plan decision support tool flyer
Employee coverage options website
Workplace communication template
3
You may have employees who waived employer-sponsored health coverage and kept their Medicaid benefits when starting employment with your company.
If these employees are disenrolled from Medicaid, they may become eligible for a special enrollment period due to what’s known as a qualifying life event. During this specified window of time, employees can enroll in a group medical plan or obtain other health coverage outside of your organization’s standard open enrollment period.1
Medicaid renewals have resumed, and millions of individuals may lose health coverage. They will need to take action to either keep their current Medicaid coverage or find a new health plan that’s right for them. There are options to make sure they stay covered and protected. We can help.
Click on the thumbnails to view the resources linked below.

1
An employee could still qualify for Medicaid benefits and maintain their coverage. Employees may take steps to renew coverage with their state agency.
2
An employee may no longer qualify for Medicaid benefits and could join your employer-sponsored group plan.
3
An employee may not qualify for either Medicaid or your group plan, but could enroll in an Anthem Individual and Family Plan through the Health Insurance Marketplace® or their state exchange.
Your employees have options for health insurance if they don’t qualify for your employer group plan. Our decision support tool can help them find the right health plan. The tool also offers personalized guidance by matching an employee to state and federal benefits they may qualify for, including food, housing, and child care programs.
With the restart of Medicaid eligibility reviews, Bill is notified that he is no longer eligible for Medicaid as his income has changed.
Bill was hired as a part-time employee and not eligible for employer-sponsored coverage. Bill has diabetes, and having health coverage to manage his condition is important. He enrolled in Medicaid at a time when state eligibility reviews were paused. Now his position has been moved to full-time status.
Bill relies on his diabetes management plan with his doctor, and staying covered is important to him. He reaches out to his company’s Human Resources (HR) department to discuss his plan options.
HR provides Bill coverage options to help determine what plan is best for him. He can choose to either enroll in his company’s group health plan or opt for an Anthem Individual and Family plan through the federal Health Insurance Marketplace or his state exchange.
Bill decides to join his company’s employer-sponsored health plan. Since losing Medicaid coverage is a qualifying event with a special enrollment period, Bill is eligible to sign up during that period.

Learn about the decision support tool here.


Making sure all of your employees are covered shows you support them prioritizing their health, and healthy employees are more focused and productive at work.


Employee coverage options flyer
Employee resources flyer
Printable information flyer
Health plan decision support tool flyer
Employee coverage options website
Workplace communication template
Your employees are the heart of your organization. As your trusted health partner, we can help you make sure they have the information they need to maintain health benefits and navigate changes in Medicaid coverage.


1 Guidance may be issued at a later date extending the Special Enrollment Period in some circumstances.
2 Gallop®: Leaders: Ignore Employee Wellbeing At Your Own Risk (accessed September 2023): gallop.com.
3 Bill’s story represents a potential member journey and is hypothetical in nature.
4 The White House: Fact Sheet: Biden Harris Administration Proposes Rule to Fix “Family Glitch” and Lower Health Care Costs (accessed October 2022): whitehouse.gov.
Anthem Blue Cross and Blue Shield is the trade name of: In Colorado: Rocky Mountain Hospital and Medical Service, Inc. HMO products underwritten by HMO Colorado, Inc. In Connecticut: Anthem Health Plans, Inc. In Indiana: Anthem Insurance Companies, Inc. In Georgia: Blue Cross Blue Shield Healthcare Plan of Georgia, Inc. and Community Care Health Plan of Georgia, Inc. In Kentucky: Anthem Health Plans of Kentucky, Inc. In Maine: Anthem Health Plans of Maine, Inc. In Missouri (excluding 30 counties in the Kansas City area): RightCHOICE® Managed Care, Inc. (RIT), Healthy Alliance® Life Insurance Company (HALIC), and HMO Missouri, Inc. RIT and certain affiliates administer non-HMO benefits underwritten by HALIC and HMO benefits underwritten by HMO Missouri, Inc. RIT and certain affiliates only provide administrative services for self-funded plans and do not underwrite benefits. In Nevada: Rocky Mountain Hospital and Medical Service, Inc. HMO products underwritten by HMO Colorado, Inc., dba HMO Nevada. In New Hampshire: Anthem Health Plans of New Hampshire, Inc. HMO plans are administered by Anthem Health Plans of New Hampshire, Inc. and underwritten by Matthew Thornton Health Plan, Inc. In 17 southeastern counties of New York: Anthem HealthChoice Assurance, Inc., and Anthem HealthChoice HMO, Inc. In these same counties Anthem Blue Cross and Blue Shield HP is the trade name of Anthem HP, LLC. In Ohio: Community Insurance Company. In Virginia: Anthem Health Plans of Virginia, Inc. trades as Anthem Blue Cross and Blue Shield, and its affiliate HealthKeepers, Inc. trades as Anthem HealthKeepers providing HMO coverage, and their service area is all of Virginia except for the City of Fairfax, the Town of Vienna, and the area east of State Route 123. In Wisconsin: Blue Cross Blue Shield of Wisconsin (BCBSWI) underwrites or administers PPO and indemnity policies and underwrites the out-of-network benefits in POS policies offered by Compcare Health Services Insurance Corporation (Compcare) or Wisconsin Collaborative Insurance Corporation (WCIC). Compcare underwrites or administers HMO or POS policies; WCIC underwrites or administers Well Priority HMO or POS policies. Independent licensees of the Blue Cross and Blue Shield Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc.
1044513MUEENABS Rev. 2/24

3